AHL Newsletter December 2018
Click here for a pdf copy of the December 2018 AHL Newsletter.
AHL Holiday Hours, 2018/19
 Season's Greetings from the staff of the animal Health Laboratory
Season's Greetings from the staff of the animal Health Laboratory
Except for closure on Christmas Day, Dec 25, the AHL is open every day with limited services; the U of Guelph is officially closed Saturday, Dec 22 through Tuesday, Jan 1, 2019.
Guelph – Usual Saturday services = specimen reception, emergency mammalian PMs, full bacteriology set-up, as well as clinical pathology testing.
Guelph - Statutory holiday services and usual Sunday services include: specimen receiving, emergency mammalian PMs, and bacteriology set-up.
AHL-Kemptville - open December 24, 27, 28, and 31.
Guelph and Kemptville drop box and/or fridges are available 365/24/7 for specimen drop off.
For full details, please see our website – www.ahl.uoguelph.ca
Cold weather shipping reminder
Jim Fairles
It’s that time of year again when we need to start thinking about preventing samples from freezing. Specimens such as EDTA blood are rendered useless when frozen. Formalin will also freeze, which creates artifacts in fixed tissue. It can be difficult to protect samples shipped during the winter from severe cold. Even 10% neutral-buffered formalin will freeze in harsh winter weather conditions. To inhibit or reduce formalin freezing, add 1 mL of ethanol per 10 mL of formalin. Samples that should not be frozen should
be shipped inside insulated containers with minimal cold packs. Use of room temperature cold packs will help prevent temperatures from dipping too low. If you have any concerns about the best way to ship critical samples, please contact the AHL. ahlinfo@uoguelph.ca
Fish testing is expanding at the AHL
The AHL established a fish testing section in 2014, under the leadership of Dr. Hugh Cai. Since then, we have tested a wide range of samples covering disease diagnosis and surveillance, health checks, fish movement certification and fish export certification, and have reported several CFIA reportable diseases. Recently, Dr. Heindrich Snyman joined the AHL in Kemptville. Dr. Snyman has 5 years experience in fish pathology and he will deal with histopathology for research fish and aquarium fish and provide case coordination. Dr. Nikki LePage will continue as our consulting fish pathologist with a focus on commercial aquaculture fish. The AHL fish lab test spectrum includes:
* Gross and histopathology.
* Gill and skin scraping wet mount microscopy examinations.
* Bacterial culture and antimicrobial resistance testing, MALDI-TOF MS and DNA sequencing.
* PCR for infectious salmon anemia virus (ISAV), Koi herpesvirus (KHV), infectious hematopoietic necrosis virus (IHNV).
* PCR for viral hemorrhagic septicemia virus (VHSV), Myxobolus cerebralis (whirling disease pathogen). Both tests are ISO 17025:2005 accredited, as shown by the scopes posted on our website. AHL
Premises ID and Client Portal
Jim Fairles, Josie Given
In partnership with OMAFRA, the Animal Health Laboratory is now offering to help facilitate veterinary clinics and their clients in obtaining their Premises ID (PID). A single agreement with AHL is to be signed by the clinic stating that any premises information provided to the laboratory was done with the client’s consent. Together, we can work to quickly and efficiently get the PID numbers added to your client database. Once the client has been assigned a PID, a PPR certificate will be either emailed (preferred) or sent by mail to the owner of the premises.
AHL is now rolling out a Client Portal. Once your client PIDs are obtained, using the portal will standardize your diagnostic submissions (spelling of owner names, PID, farm name, trending, etc.)
Þ Create your submissions online, in-clinic, ensuring proper spelling, PIDs and demographics.
Þ Track the progress of your cases, edit/cancel up until the specimen is received at AHL.
Þ Advanced search capabilities, design reports based on Animal ID, farm, owner, etc.
Þ Know your case # prior to sending to AHL, track its progress as results are made available.

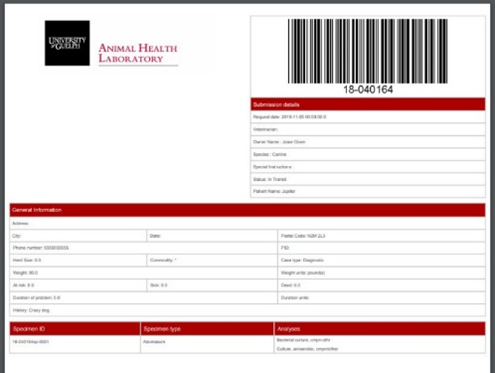
Contact Josie Given: 519-824-4120 ext 54320, or jgiven@uoguelph.ca to setup a training session today!
AHL Newsletter December, 2018 - Volume 22, Number 4
Editor: Grant Maxie, DVM, PhD, Diplomate ACVP
Editorial Assistants: Helen Oliver, April Nejedly
The AHL Newsletter is published quarterly (March, June, September, December) by the Animal Health Laboratory, Laboratory Services Division, University of Guelph.
Its mission is to inform AHL clients and partners about AHL current activities, and laboratory-based animal disease events and disease trends. All material is copyright 2018. Ideas and opinions expressed herein do not necessarily reflect the opinions of the University or the Editor.
Articles may be reprinted with the permission of the editor and with appropriate credit given to the AHL Newsletter.
Mailing address & contact information:
Animal Health Laboratory
Laboratory Services Division, University of Guelph
Box 3612, Guelph, Ontario, Canada N1H 6R8
Phone: (519) 824-4120 ext. 54538; fax: (519) 821-8072
To receive an electronic copy of this Newsletter, please send your email address to us at holiver@uoguelph.ca
ISSN 1481-7179
Canada Post Publications number - 40064673
Contributors to this issue
- from the Animal Health Laboratory:
Marina Brash, DVM, DVSc, Diplomate ACVP
Andrew Brooks, DVM, PhD, Diplomate ACVP
Hugh Cai, DVM, MSc, DVSc
Michael Deane, BA
Josepha DeLay, DVM, DVSc, Diplomate ACVP
Jim Fairles, DVM, MBA
Josie Given, BA
Murray Hazlett, DVM, DVSc, Diplomate ACVP
Amanda Mansz, DVM, DVSc, Diplomate ACVP
Emily Martin, DVM, MSc, Diplomate ACPV
Felipe Reggeti, DVM, PhD, Diplomate ACVP
Kris Ruotsalo, DVM, DVSc, Diplomate ACVP
Nick Schrier, MSc
Durda Slavic, DVM, PhD
Maria Spinato, DVM, DVSc, Diplomate ACVP
Margaret Stalker, DVM, PhD, Diplomate ACVP
Kate Todd, DVM
Other contributors:
Luis G Arroyo LicMedVet., DVSc, PhD, DACVIM, Clinical Studies; Janet Beeler-Marfisi, DVM, DVSc, DACVP; Nancy Brochu, DVM; Brandon Lillie, DVM, PhD, DACVP; Christina McKenzie, BSc, DVM; Leonardo Susta, DVM, PhD, DACVP; Pathobiology, Michele Guerin, DVM, PhD, Population Medicine; OVC
Tim Blackwell, DVM, PhD; Csaba Varga, DVM, PhD; Andrew Vince, DVM, DVSc, Diplomate ACVP, OMAFRA
Talia Fletcher, DVM, Markdale, ON
Diana Gibbs, DVM, MSc, Burlington, ON
Mike Krystolovich, DVM, Guelph, ON
Rainee Stoddart, DVM, Barrie, ON
Our continued thanks to all of the non-author AHL clerical, technical, and professional staff who contribute to the generation of results reported in the AHL Newsletter.
Ontario Animal Health Network
Your comprehensive source for animal health information.
OAHN Update - December 2018
Dr. Kate Todd joined OAHN in October as the Network Coordinator, covering for Dr. Melanie Barham while she is on maternity leave. Kate is a DVM 2007 graduate of OVC, originating from Stratford, ON. Following graduation, she pursued mixed animal practice (with a focus on equine/small animal medicine) near her home town. She has since worked throughout Canada as a locum, as far west as B.C. and Alberta, and as far east as Newfoundland. She has a particular interest in imaging and internal medicine, and completed courses in ultrasonography as an adjunct to practice. She brings her enthusiasm and ideas to continue to build the OAHN expert networks, and works to strengthen ties among producers, industry, and veterinary practitioners, and to effectively communicate disease surveillance information.
The network co-leads participated in a training session on Nov. 14, facilitated by Evalina Rog and Linda Watt of the University Learning and Development Centre. This sparked some interesting discussions and thoughts about cooperation, coordination, and collaboration, and how we can involve network participants in planning for projects and activities.
OAHN Annual Workshop
On Nov. 21, the OAHN Annual General Meeting was held at the Ignatius Jesuit Centre in Guelph. A total of 70 network members, government, and industry representatives attended the meeting. Dr. Davor Ojkic and Dr. Jim Fairles spoke on the topic of "Evolution of animal health testing in the molecular age" as the keynote presentation for the session. The networks shared information and successes of 2018, and participated in a planning session to establish their network goals and projects for 2019.
African Swine Fever Infographics
 The OAHN Swine Network created 2 infographics covering African Swine Fever Prevention Tips. These infographics cover signs of ASF illness, as well as emphasizing making herd health and biosecurity a priority. You can find these infographics here: https://oahn.ca/news/african-swine-fever-prevention-infographics/. Ontario Pork was able to distribute these infographics to more than 4,000 backyard swine producers throughout Ontario.
The OAHN Swine Network created 2 infographics covering African Swine Fever Prevention Tips. These infographics cover signs of ASF illness, as well as emphasizing making herd health and biosecurity a priority. You can find these infographics here: https://oahn.ca/news/african-swine-fever-prevention-infographics/. Ontario Pork was able to distribute these infographics to more than 4,000 backyard swine producers throughout Ontario.
Varroa Mite Awareness Campaign for Ontario Beekeepers
Throughout the end of August and the beginning of September, OAHN joined with some of Ontario’s top beekeepers to lead FREE workshops teaching Ontario beekeepers about how to test for Varroa mites in their hives. We then collected data from Ontario beekeepers, and mapped these data. Find out everything about this project here: https://oahn.ca/resources/oahns-varroa-mite-awareness-campaign/

New Podcast and Reports
The OAHN Companion Animal Network has put together a new podcast with Dr. Bronwyn Rutland on Chronic Diarrhea in Dogs and Cats. Dr. Rutland and OAHN Companion Animal Network co-lead Dr. Maureen Anderson discuss chronic diarrhea in dogs and cats. They discuss what chronic diarrhea is, common causes, infectious diseases, management strategies (including fecal transplantation), diagnostic approaches, and much more. You can access it at the OAHN Podcast Page: http://oahn.podbean.com/
We have lots of new reports, lab data, and resources. Be sure to check out OAHN.ca
Improving the success rate of abortion diagnosis
Josepha DeLay, Murray Hazlett, Maria Spinato, Andrew Brooks, Jim Fairles
Identifying the cause of abortion in domestic animals is important so that measures can be taken to prevent additional losses and avoid significant economic impact at the herd or flock level. However, determining the exact cause of abortion can be a frustrating process for veterinarians, producers / owners, and veterinary pathologists. Some cases are the result of physiologic, hormonal, genetic, or other causes that may not produce morphologic lesions or be detectable by available diagnostic tests. Although the cause of abortion is unknown (idiopathic) for a proportion of abortions in all species, a routine approach to testing often allows at least broad categorization of the cause as infectious vs. non-infectious, and exclusion of many specific infectious agents.
The thoroughness of tissue sampling and diagnostic testing has a significant impact on the success rate of abortion diagnosis. Fetuses and placentas submitted intact to the diagnostic laboratory are examined by pathologists in a consistent manner, and a routine battery of microbiologic tests and histopathology are carried out based on the species and clinical history. This approach will identify the involvement of infectious agents and non-infectious conditions in a high proportion of cases.
We reviewed the diagnostic success rate of abortion cases by submission type, abortion submissions to the AHL from multiple livestock species in 2017 and 2018. ‘AHL postmortem (PM) submissions’ included those for which 1 or more fetuses, with or without placenta, were submitted for examination and diagnostic test selection by a pathologist. ‘Field / in-clinic postmortem (PM)’ submissions included those for which PM exam, sampling, and test selection was carried out by veterinary practitioners. Submissions for full PM by a pathologist made up the majority of abortion cases submitted to the AHL (Fig. 1). In all species, the frequency of a definitive or suspected (histologically compatible) etiologic diagnosis was higher for AHL PM submissions than for those cases in which samples were collected by field or in-clinic PM (Fig. 2). All swine abortion cases were submitted as AHL PM submissions, precluding comparison of results based on submission type for this species.
The advantage of a consistent, standardized approach to diagnostic testing of abortion cases is illustrated by these results. To increase the diagnostic success rate for abortion cases, veterinarians are encouraged to submit fetuses with placentas to the diagnostic laboratory for examination and testing. Alternatively, practitioners performing field or in-clinic PMs on abortion cases should conduct thorough exams with consistent sample collection and testing.
Recommended testing schemes for abortions in all species are listed in the AHL User’s Guide, available in print and online at https://www.uoguelph.ca/ahl/abortion . For cattle (and soon to follow for other species), more detailed information including sampling templates can also be found on the AHL website: https://www.uoguelph.ca/ahl/bovine-abortion-diagnostic-plan-april-1-2018 . Veterinarians must also be aware of the risk of zoonotic disease transmission when performing field or in-clinic PMs, especially ovine, caprine, and bovine abortions, and appropriate safety precautions should be taken.
There is justifiable concern about the cost of carrying out a set panel of diagnostic tests on every abortion case, and indeed some judicious test selection can be used in specific cases depending on the herd situation. However veterinarians and producers must also consider the financial cost of not reaching a diagnostic conclusion.

Figure 1. AHL abortion submissions by species and sample type, 2017-2018: AHL PM vs. field / in-clinic PM (%).

Figure 2. Frequency of definitive or suspected abortion diagnoses by submission type, 2017-2018: AHL PM vs. field/in-clinic PM (%).
RUMINANTS
What’s your diagnosis?
Josepha DeLay, Felipe Reggeti, Mike Krystolovich

Stillborn Holstein calf with disproportionate dwarfism (note proportionately shortened limbs, compared to body), hindlimb arthrogryposis, lumbar kyphosis, and shortened maxilla). Dam was a first-calf heifer in poor body condition.
Answer:
Disproportionate dwarfism is a hallmark of congenital nutritional chondrodystrophy associated with maternal micronutrient deficiency during gestation. Manganese deficiency is recognized as a cause of this condition. Liver manganese levels in this fetus were low (0.77 µg/g; ref. 2.0-6.0 µg/g for adult cattle), although manganese levels typically do not reach the adult range until 2-3 wk of age. Further work is needed to determine the normal range of liver manganese in Ontario calves and fetuses.
Disproportionate dwarfism associated with manganese deficiency has been described in calves in Canada, New Zealand, and elsewhere. Joint laxity and swelling is also documented in some affected animals. Low manganese levels in feed have been linked to drought conditions during the previous growing season, as well as to diets inherently low in manganese, including unsupplemented corn silage.
Manganese contributes to pathways of glycosaminoglycan synthesis, and deficiency of this essential micronutrient disrupts normal endochondral ossification and bone development. Kyphosis in this fetus was related to malformation of lumbar vertebrae, suspected to also be associated with micronutrient deficiency here. Resulting spinal cord compression was the likely cause of concurrent arthrogryposis. AHL
References
McLaren PJ, et al. Chondrodysplastic calves in northeast Victoria. Vet Pathol 2007;44:42-354.
Puls R. Mineral Levels in Animal Health. Clearbrook, BC:Sherpa International, 1994.
Ribble CS, et al. Congenital joint laxity and dwarfism: a feed-associated congenital anomaly of beef calves in Canada. Can Vet J 1989;30:331-338.
White PJ, Windsor PA. Congenital chondrodystrophy of unknown origin in beef herds. Vet J 2012;193:336-343.
Copper toxicosis in a dairy goat herd
Murray Hazlett, Talia Fletcher, Felipe Reggeti
A dairy goat herd of ~100 animals experienced 10 sick and 10 dead animals. For the previous 8 mo, the owner reported problems with the doelings that appeared to wax and wane. The goats would go off feed and then deteriorate rapidly. To investigate, a 4-mo-old goat that had recently died was autopsied. It was weak and paddling before death with a mild fever (39.6oC) and died about 2 h after the producer noticed clinical signs. It had a body condition of 3/5, was mildly dehydrated, and had normal fat and muscle stores. There was pulmonary congestion. Polioencephalomalacia or listeriosis was suspected, and fixed and fresh tissue samples were submitted to the AHL for testing.
Histology showed dissociation of hepatic cords with single-cell necrosis (Fig. 1) and mild diffuse increase in leukocytes in hepatic sinusoids. In brain, there was cerebral cortical edema with the presence of cells compatible with Alzheimer type II cells – these cells are formed usually in the face of liver or colonic damage, and are associated with hyperammonemia. Because of the liver lesions, copper analysis was done on liver, which had levels of 270 µg/g (reference interval [RI] 25 - 150 µg/g) and kidney which had levels of 96 µg/g (RI 3.0 - 6.0 µg/g).
Toxicology results in this case indicate copper toxicosis. In a relatively recent report of copper toxicosis in dairy goats,1 copper levels in liver and kidney were similar to our case; hepatic necrosis without hemolysis was the main lesion.
After identification of the problem, the producer reported that both the mineral mix and the pelleted feed had been copper supplemented and that the problem resolved after correcting for this.
A 10-yr computer search of AHL pathology records for copper toxicity in goats revealed 11 cases (Table 1). In those cases which had both liver and kidney tested, it can be seen that commonly the relative increase in kidney copper compared to normal levels is much more striking that that seen in liver, which is why diagnosticians commonly prefer to test both of these organs. Hemolysis and jaundice are sometimes, but not always, seen. AHL
Reference
1. Cornish J, et al. Copper toxicosis in a dairy goat herd. J Am Vet Med Assoc 2007;231:586-589.

Figure 1. Liver, with necrosis of individual hepatocytes (arrows).
Table 1. AHL pathology cases of copper toxicosis in goats.
|
Breed |
Age |
History |
Submission diagnosis |
Liver Cu (25-150 µg/g) |
Kidney Cu (3-6 µg/g) |
|
Goat |
|
None given. |
Acute hepatic necrosis due to Cu toxicity |
1,267 |
- |
|
Goat |
|
Diarrhea. |
Hepatopathy with nephrosis - r/o Cu |
- |
- |
|
Saanen |
1.5 y |
Sudden death. |
Acute hepatic necrosis |
|
|
|
Pygmy goat |
2 y |
Weak. |
Hepatopathy with elevated renal Cu levels |
170 |
48 |
|
Boer goat |
3 y |
Sudden death. |
Hepatic single cell necrosis - compatible with Cu toxicosis |
350 |
- |
|
Nubian |
3 y |
Sick 8 days. Liver orange. |
Hepatopathy - bile stasis and hemoglobinuric nephrosis |
190 |
31 |
|
Goat |
3.2 y |
Sick one day, down in sternal recumbency. |
Acute hepatic necrosis |
330 |
150 |
|
Mixed-breed goat |
4 mo |
Sudden death. Weak. Paddling, pupils unresponsive. |
Acute hepatic necrosis - Cu toxicosis |
270 |
96 |
|
Saanen |
2.5 mo |
Didn't eat. Ran away when treated. Dead next day. |
Periacinar hepatic necrosis - Cu toxicosis |
360 |
190 |
|
Caprine |
2 y |
Found dead. Kidded 2 mo ago. |
Nephropathy - probable Cu toxicosis |
- |
- |
|
Toggenburg |
7 mo |
Separated from rest of herd. Given horse feed. |
Hepatic necrosis due to Cu toxicosis |
478 |
114 |
SWINE
Mycobacterial lymphadenitis in market hogs
Josepha DeLay, Jim Fairles, Durda Slavic, Hugh Cai, Amanda Mansz, Margaret Stalker, Tim Blackwell, Andrew Vince
Enlarged mesenteric and mandibular lymph nodes with grossly visible caseous granulomas were identified at slaughter in several market hogs originating from 3 Ontario herds. Histologic evaluation confirmed granulomatous and pyogranulomatous necrotizing lymphadenitis (Fig. 1). Low numbers of acid-fast bacilli compatible with mycobacteria were visible in direct smears or histologic sections from ~ 50% of affected nodes (Fig. 2). Mycobacterium avium (not speciated) was isolated by Public Health Agency Ontario Laboratories from one of the lymph nodes.
Investigation of the source herds confirmed that the herds had fed peat moss as a supplement to nursing or weaned pigs. In young pigs, peat feeding has been associated with improved growth and performance, purportedly due to stabilizing effects on intestinal microflora, micronutrient supplementation (including iron), and adsorption of potentially toxic substances (such as bacterial toxins). Peat is an interesting substance that forms naturally through sedimentation of organic debris in cold, wet, anaerobic environments, which limit decomposition. “Peat” or “peat moss” is composed primarily of decomposing wetland/bog flora, usually including Sphagnum spp. mosses but often many other species of plants, particularly if harvested from natural bogs, and is sold in North America primarily as a horticultural soil supplement. In addition to the predominant organic content, peat also contains inorganic compounds and microorganisms in a heterogeneous mix dependent on the geographic location of the source. Inherent risks in peat exposure are recognized as a result of these natural contaminants. Open, outdoor post-harvest storage of peat provides additional opportunities for contamination. Environmental conditions facilitating peat formation are also favorable for mycobacterial growth. Lymphadenitis in swine due to opportunistic infection with M. avium (predominately M. avium ssp. hominissuis) has been reported as a complication of peat exposure.
Lymphadenitis, including mycobacterial lymphadenitis, can result in partial or complete carcass condemnation at slaughter and associated economic losses for producers. Human infection with M. avium is also possible, and the potential for clinical disease is highest in young or immunocompromised individuals. AHL
References
Johansen TB, et al. Mycobacterium avium subsp. hominissuis infection in swine associated with peat used for bedding. BioMed Res Intern 2014. doi: 10.1155/2014/189649. Epub 2014 Sep 15.
Ontario Ministry of Agriculture, Food, and Rural Affairs. Peat moss for piglets at weaning (factsheet). 2012. http://www.omafra.gov.on.ca/english/livestock/swine/facts/info_n_peatmoss.htm
Trckova M, et al. Peat as a feed supplement of animals: a review.

Figure 1. Mandibular lymph node, market hog. Normal node architecture is replaced and effaced by caseous granulomas. H&E stain, 200x.

Figure 2. Mandibular lymph node, market hog. A few acid-fast bacilli (circled) among central debris in caseous granuloma. Ziehl-Neelsen acid-fast stain, 1000x.
AVIAN/FUR/EXOTIC SPECIES
Disease surveillance of Ontario small flocks – update
Leonardo Susta, Nancy Brochu, Michele Guerin, Csaba Varga, Brandon Lillie, Marina Brash
The prospective pathogen surveillance study carried out by the AHL and Pathobiology regarding small flocks (non-quota / non-commercial) has come to an end. The study ran from October 1st 2015 until September 29th 2017, and sought to determine the baseline prevalence of relevant infectious agents and diseases in postmortem submissions from Ontario small flocks. For a substantially discounted fee of $25.00 per submission, owners were encouraged to submit sick or dead birds (through their veterinarian) to the AHL locations in Guelph or Kemptville for postmortem examination and a pre-set array of microbiologic tests (conducted on all birds, regardless of lesions).
We received 160 submissions, for a total of 245 individual birds. Most submission derived from southwestern and eastern Ontario. Eighty-four percent of submissions were chickens, followed by turkeys (10 submissions), game birds (8 submissions), and ducks (8 submissions). As reported by the owners in the submission history, affected flocks ranged from 1-299 birds.
No federally reportable diseases were detected. A vaccine strain of avian avulavirus-1 (AAvV-1, formerly known as Newcastle disease virus), and a low pathogenic (H10N8) avian influenza A virus (AIV) isolate were detected in one chicken and one turkey submission (out of 160 tested), respectively. No lesions were associated with these viruses. Infectious laryngotracheitis virus (ILTV) was detected in 22 submissions (34 birds), and concurrent disease (e.g., presence of syncytia, intranuclear inclusion bodies, and tracheitis) was observed in 21 chickens. Salmonella spp. was detected in the cloacal swabs of 3 chickens (S. Anatum, S. Indiana, S. Ouakam), one turkey (S. Uganda), and one duck submission (S. Montevideo); no lesions consistent with salmonellosis were identified (subclinical infection).
The most frequently identified bacterial agents were Brachyspira spp. (37%, cloacal swabs, all species), Mycoplasma synoviae (MS, 36%, tracheal swabs, all species), Campylobacter spp. (35%, cloacal swabs, all species), Mycoplasma gallisepticum (MG, 23%, tracheal swabs, all species) (Fig. 1). No Mycoplasma iowae or meleagridis were identified.
The most frequently identified viral agents were infectious bronchitis virus (IBV, 39%, tracheal and cloacal swabs, chickens and gamefowl), fowl adenovirus (FadV, 35%, cloacal swabs, chickens), ILTV (15%, tracheal swabs, chicken and gamefowl), avian reovirus (4%, cloacal swabs, chickens and turkeys), and infectious bursal disease virus (IBDV, 1%, cloacal swabs, chickens) (Fig. 2). No avian bornavirus was detected. No gross or microscopic lesions consistent with infection with Brachyspira spp., Campylobacter spp., FAdV, reovirus, or IBDV were identified (subclinical infection).
Multiple respiratory pathogens were often detected in the same submission; 44 chicken submissions were positive for >1 respiratory pathogen. The most commonly detected pathogen combinations included MG, MS, and IBV (9%); MS and IBV (8%); MG and MS (4%); and MG, MS, and ILTV (3%). When considering single birds, infection caused by mixed respiratory infections was the most common cause of mortality (21% of tested birds). At the discretion of the pathologist assigned to the case, birds diagnosed with mixed respiratory infection were also tested for bacterial isolation; the most commonly isolated bacteria were Avibacterium spp., E. coli, and Gallibacterium spp.
The single most common viral cause of death was Marek’s disease (26 chickens), which was identified by pathognomonic lymphoid infiltrate of nervous tissue, especially peripheral nerves. The most common neoplastic diseases included ovarian adenocarcinoma with celomic spread (20 birds).
Although tested flocks did not appear to be a reservoir of federally reportable diseases, mixed respiratory pathogens were commonly detected in these flocks and were considered to be the leading cause of clinical signs / poor-doing. Frequent detection of ILTV and IBV underscores the importance of implementing adequate biosecurity practices by small flock owners. Detection of mycoplasma and Marek’s disease stresses the importance of purchasing chicks or ready-to-lay pullets from reputable sources (e.g., from hatcheries or co-ops), in order to obtain replacement chicks that are free of vertically transmissible pathogens, and that are properly vaccinated (at least for Marek’s disease).
Our study provides useful baseline information on the prevalence of pathogens and diseases in small flocks in Ontario for future prevalence studies. These data will contribute to producing knowledge translation publications for specialized training regarding poultry medicine aimed at Ontario veterinarians with an interest in small poultry flock medicine, as well as developing educational tools for small flock producers aimed at prevention and control of relevant diseases. AHL

Figure 1. Prevalence (%) of bacterial pathogens in tested submissions.

Figure 2. Prevalence (%) of viral pathogens in tested submissions.
OAHN small flock poultry online veterinary course: (FREE!) Veterinarians may access this course and associated resources by logging in to www.oahn.ca (obtaining an account is free and easy). Then click this link to access the recorded lectures from this 1-day course. http://oahn.ca/resources/poultry/small-poultry-flock-workshop-for-veterinarians-presentations-live-video-and-resources/
Campylobacter hepaticus hepatitis (spotty liver disease) recently reported in American conventionally housed layers
Marina Brash, Durda Slavic
Spotty liver disease (SLD) was initially reported in laying hens raised in free-range and floor housing systems in Great Britain and Australia in the late 1990s and early 2000s. Reported clinical signs included enteritis, mortality, drop in egg production, and characteristic multifocal hepatitis (Fig. 1). Recently, SLD was reported in a large cage-raised layer complex in the United States, although there were earlier verbal communications of caged layers as well as broiler breeders and broilers, being very occasionally affected. This condition has never been confirmed in Ontario to our knowledge, but with the egg and meat bird industries undergoing dramatic housing and management changes, we need to continue to monitor mortality in our flocks for the presence of this newly emerging pathogen.
We want to remind the Ontario practitioners that the isolation of this novel Campylobacter sp. from affected tissues requires special enrichment and culture media as well as longer incubation times and these protocols were implemented a few years ago at the AHL. Based on recent information, bile is considered to be the best sample to submit for bacterial culture for Campylobacter hepaticus.
If white spotted livers are identified in any type of chicken and you wish to test for the presence of C. hepaticus, we request that you submit a fresh sample of liver that includes the intact gallbladder containing bile (Fig. 2). Routine bacterial culture will be conducted on the liver sample and only bile will be tested for the presence of this novel Campylobacter sp., if specifically requested under special instructions on the AHL submission form. In addition, please provide postmortem findings including the identification of white spotty livers and ensure the commodity class is correctly selected on the AHL submission form because only chicken bile will be tested for C. hepaticus. Regular bacterial culture charges will apply.

Figure 1: Characteristic gross liver lesions of spotty liver disease. Photos courtesy of Dr. Kelli H. Jones, CEVA.

Figure 2. Liver, including intact gallbladder containing bile, is the preferred sample for C. hepaticus culture.
Gastric neuroendocrine carcinoma in a 2-year-old bearded dragon
Emily Martin, Diana Gibbs
A 2-y-old male bearded dragon presented to the AHL for postmortem examination. There was a history of a mild decline in appetite starting early August progressing to anorexia by August 15. After 7-10 days, daily oral water therapy was started and the UVB lamp was changed (previous lamp installed January 2018). Fresh greens and vegetables or fruit were offered daily (mostly lettuce or spinach, peppers, plums, etc.). Mealworms and crickets were fed every third day (crickets gut loaded with vegetable and dusted with calcium). At 14 days, SQ fluids were administered and lab tests were run including a fecal float and radiographs. The radiographs were unremarkable and the fecal flotation revealed multiple parasites (a few Oxyurid eggs, occasional Entamoeba hartmanni-like cysts, a few trichomonad trophozoites, a few Chilomastix sp. cysts). Metronidazole treatment was started and began spoon-feeding Repashy Grub Pie daily. Over the clinical course, there was a weight loss of 33 g. On the evening of September 18, he was found unresponsive in his tank. He was brought to the AHL the next day for postmortem examination.
The most striking finding was the markedly enlarged liver with rounded borders and multifocal-to-coalescing tan nodules throughout the parenchyma, from pinpoint to 2 x 2 x 3 cm (Fig. 1). On cut section, the nodules were tan-yellow with firm consistency throughout or occasionally pale-pink with soft centers (Fig. 2). The remaining hepatic parenchyma was tan-green and the gallbladder was markedly distended. There was also a 1 cm x 3 mm firm cream mass within the stomach wall.
On histopathology of the liver, small-to-large, multifocal-to-coalescing masses expanded and replaced the normal architecture of the liver. Within these masses were neoplastic cells variably arranged in packets, acini, and trabecular cords separated by fine fibrous vascular stroma (Fig. 3). The cells had round euchromatic nuclei and scant cytoplasm. Within the masses, the neoplastic cells ranged from monomorphic populations at the margins to anaplastic populations with marked nuclear polymorphism in the center. The stomach metastatic gastric mass extended through the gastric mucosa and submucosa (Fig. 4). There was also evidence of vascular invasion.
The morphology of the mass was consistent with gastric neuroendocrine carcinoma. This is a neoplasm that has been described in young bearded dragons as highly malignant and readily able to metastasize. This tumor should be considered as a rule-out in cases of young bearded dragons (< 3-y-old) with clinical signs of anorexia, weight loss, weakness, or vomiting. AHL
References
Lyons JA. A gastric neuroendocrine carcinoma expressing somatostatin in a bearded dragon (Pogona vitticeps). J Vet Diagn Invest 2010;22:316–320.
Ritter JM, et al. Gastric neuroendocrine carcinomas in bearded dragons (Pogona vitticeps). Vet Pathol 2009;46:1109–1116.

Figures 1-4. Neuroendocrine carcinoma in a bearded dragon. Figure 1, 2. Ventral surface and cut surface of liver. Figures 3, 4. Hepatic nodule. Gastric mass. H&E. 20X.
HORSES
Cutaneous angiomatosis (a.k.a. lymphangioma, lymphangiomatosis) in a young horse
Murray Hazlett, Christina McKenzie, Rainee Stoddart, Luis G. Arroyo
A 3-y-old warmblood mare was presented with a history of intermittent swelling and discharge on the skin over the gluteal area, on both sides, mainly in the right side. The masses were 5-20 mm small soft skin bumps and were felt to be multilocular cysts that would periodically drain (Fig. 1A). The mare was biopsied on the farm.
The biopsy was diagnosed as a cutaneous lymphangioma (Figs. 1B, C). Because of the lack of blood present in the spaces, it was suspected these were lymphatic vessels. No mitotic figures were seen. Cellular pleomorphism was minimal. The horse was referred to the Ontario Veterinary College for additional workup and re-biopsy. The second biopsy was similar, with all layers of the dermis and the dense subcutaneous collagen, hair follicles, and dermal collagen separated by elongated, clear spaces lined by a single layer of inconspicuous endothelium and that wrapped around pre-existing collagen bundles resulting in a short branching pattern. Some lumina contained moderate numbers of red blood cells (interpreted as blood and/or lymphatic vessels). In the dermis, the clear spaces were mostly arranged parallel to hair follicles and extended to the epidermis. Endothelial cells lining these dilated vessels were flattened, with minimal cytoplasm and basophilic nuclei with inconspicuous nucleoli, and they stained positive for factor VIII (Fig. 1D) – an endothelial cell marker. No mitotic figures were seen.
Nomenclature used for this lesion varies in the literature, usually referring to equine cutaneous lymphangioma. It is questionable as to whether lymphangiomas are “true” neoplasms or hamartomas, i.e. a tumour-like proliferative disease originating from altered fetal development of the lymphatic system. Lymphangiomas occur predominantly at locations where the lymphatic system develops primitive lymph sacs – the jugular and inguinal lymph sacs, existing in pairs, and the retroperitoneal lymph sac and the cisterna chyli* (Bachmann and Worm 1967). This would explain the common distribution of these lesions in humans, where they are better documented, on the neck, axilla, retroperitoneal tissue, thighs and inguinal regions. It would also explain the bilateral distribution of the lesions seen in this horse. Fetal tissue growth and changes may result in isolated non-communicating lymphatic tissue that proliferates. Therefore, this neoplasia is observed predominantly in young individuals.1
The horse was not treated and treatment regimens are currently being decided. AHL
*Much of this work was originally done by Florence R Sabin M.D. published in 1902 – in Developmental Dynamics, Vol 1, May 1902. This meticulous work has held up for > 100 years. Dr Sabin was the first woman to hold a full professorship at Johns Hopkins School of Medicine, the first woman elected to the National Academy of Sciences, and the first woman to head a department at the Rockefeller Institute for Medical Research.
Reference
1. Gehlen H, Wohlsein P. Cutaneous lymphangioma in a young Standardbred mare. Equine Vet J 2000;32:86-88.

Figure 1. A. Gross photograph of the lesion – lumpy area on the hip region (arrow). B. Full-thickness biopsy showing vessels in the superficial and deep areas of the vessel (arrows). C. Close view of vessels in the deep layers of the biopsy. D. Factor VIII IHC stain shows red staining of cells lining the vessels compatible with vascular or lymphatic endothelium.
COMPANION ANIMALS
Confirmation of methomyl poisoning in a cat by LC-MS
Felipe Reggeti, Nick Schrier, Amanda Mansz
A 5-mo-old indoor/outdoor male DSH cat was found dead outside the owner’s house. The cat was healthy and had not received any medications or vaccines. The carcass was submitted to the AHL for postmortem examination. The body was in good condition, with adequate muscle mass and good hair coat. The stomach was filled with 40 mL of soft brown, slurry-like feed material admixed with a few grains of rice and flecks of black-brown dried leaves. The feed material within the fundus of the stomach, towards the pylorus, was discoloured aqua blue/green (Fig. 1). The remaining PM exam was unremarkable. Gastric contents were submitted to the toxicology section, and “Methomyl” was identified by LC-MS.
Methomyl (S-methyl-N-[(methylcarbamyl)oxythioacetamide]) is a broad-spectrum carbamate insecticide/acaricide. It is highly toxic to humans and animals (oral LD50 rats: 12-48 mg/kg) with anticholinesterase activity causing neurologic signs. In acute toxicity, death may result from paralysis of respiratory muscles and/or airway constriction. The product is commonly used to control flies; however, cases of misuse to intentionally kill wildlife have been reported in North America. Methomyl products typically contain the co-ingredient muscamone [(Z)-9-tricosene], a pheromone found in dipteran flies. In addition, caffeine-containing fluids are frequently added to the bait for malicious poisoning. Identification of these substances may provide clues for toxicologic investigation in some cases. The AHL offers a comprehensive GC/MS-LC-MS method for identification of over 400 pesticides - see LabNote 59 https://www.uoguelph.ca/ahl/ahl-labnote-59-gcms-lcms-multi-residue-method , as well as other potentially toxic compounds, including tremorgenic mycotoxins, strychnine, barbiturates and others; however, it cannot identify all possible toxins. Suitable samples include liver, GI contents and suspect material. Please submit frozen. AHL

Figure 1. Stomach contents of a cat poisoned with methomyl. Note the blue-green discoloration of the stomach contents.
Mycoplasma haemofelis infection in a DSH cat
Kris Ruotsalo, Janet Beeler-Marfisi
A 2-y-old, castrated male, domestic shorthaired cat was presented with a 2-d history of lethargy and pallor. Serum biochemistry and CBC revealed marked hyperbilirubinemia 139 µmol/L (reference interval [RI] 0-3 µmol/L), marked mildly regenerative anemia, hematocrit 0.10 L/L (RI 0.28-0.49 L/L), and hemoglobin 31 g/L (RI 93-153 g/L).
Blood smear examination confirmed marked anemia (Fig. 1); hemotropic mycoplasmas appear as small (0.3-0.8 µm), blue-staining cocci, rings, or rods that are usually attached to erythrocytes (partially buried in on the cell surface), or occasionally noted free within the slide backgrounds. PCR is needed for specific identification. PCR testing at the AHL confirmed the presence of M. haemofelis; M. haemominutum and M. turicensis were negative. M. haemofelis is the most pathogenic of the 3 hemotropic mycoplasmas, the least prevalent, one of the most common infectious causes of regenerative anemia in cats, and one of the causative agents of immune-mediated hemolytic anemia in cats.
A follow up CBC was taken 11 d after initial presentation and a course of treatment; hematocrit was 0.31 L/L and hemoglobin was 97 g/L, with no organisms identified on the peripheral blood smear. AHL

Figure 1. Mycoplasma haemofelis infection. Note marked anemia, RBC ghosts (intravascular hemolysis), abundant epicellular coccoid-to-signet-ring shaped organisms at the periphery of the RBCs and free in the slide background.
AHL Newsletters and LabNotes are available on the Web at - http://ahl.uoguelph.ca
 Season's Greetings from the staff of the animal Health Laboratory
Season's Greetings from the staff of the animal Health Laboratory