AHL Newsletter, September 2015
For a pdf copy of AHL Newsletter, September 2015 click here
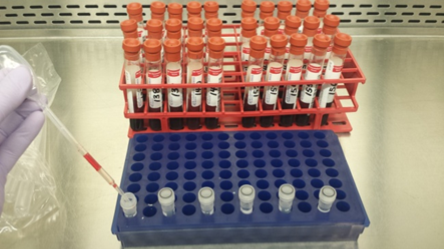
Pooling of samples for AHL testing
Joanna Sawicki
In order to control costs, samples are often pooled before testing in our microbiology labs. Individual samples can be tested should pools test positive for the agent or antibody in question. The AHL charges a cost-recovery fee for pooling of samples, but clients are welcome to pool before submitting. For details, see our new LabNote:
Briefly:
· Label all original tubes and pooling tubes in order to be able to go back and open positive pools for further testing.
· Use a new transfer pipette for each sample.
· Change gloves between cases.
· Submit to the lab ASAP.
Diagnostic dilemma!
Kris Ruotsalo
Question: What are the nucleated cells within the blood smear on the left?
|
|
|
Answer: Degenerate leukocytes!
The slide on the left was prepared from an EDTA sample that had spent 2 days in transit before reaching the AHL. The majority of the cells within the sample, and therefore within the smear, were degenerate, rendering both manual and automated leukocyte differentials, and total leukocyte count unreliable. However, as recommended, the submitting clinician had also included an air-dried, unstained blood smear (on the right) prepared at the time of blood collection. Using this well-prepared smear, we were able to provide an estimated total leukocyte count, an accurate 100 cell leukocyte differential count, an estimated total platelet count, and comment on the presence or absence of anemia.
This example serves as a reminder of the importance of always sending a well prepared, air-dried blood smear along with all EDTA blood samples, whenever a CBC is requested. This is particularly important if the sample is anticipated to spend a prolonged time in transit and during weather extremes (both hot and cold).
Job shadowing at the Animal Health Laboratory
Andrew Vince
It is rare that people are invited to see firsthand the detailed inner workings of the Pathology service at the Animal Health Laboratory. However, on May 28th, 2015, Dr. Andrew Vince invited OVC veterinary student Abby Finley to job shadow him through a full day as a diagnostic pathologist with the AHL. The day started with a brief tour through the pathology lab sections, followed by an hour observing the post-mortem dissection and sampling of a cat with subaortic stenosis. This was then followed by lunch and a discussion of the training procedures involved in becoming a veterinary pathologist. The afternoon was spent reviewing surgical pathology slides, across a breadth of different species, and discussing how we integrate histology and other ancillary tests.
Abby’s opportunity was provided through the 2015 Global Vets silent auction. Global Vets is a program at the Ontario Veterinary College that provides opportunities for veterinary students to gain experience in animal health care in developing countries. Founded in 1997, Global Vets was formed to promote international collaboration on agricultural development, animal health and welfare, and ecosystem health. The silent auction helps raise money to support second-year OVC students in traveling to various developing countries for 4-8 weeks as volunteers with ongoing veterinary-related projects aimed at improving the health and welfare of animals and people. Dr. Andrew Vince and the AHL are proud to be able to provide this opportunity for veterinary students and to help raise money for Global Vets.

OAHN Update August 2015
OAHN has had a busy quarter, with the launch of our official webpage at http://oahn.ca, the release of many new podcasts at http://oahn.podbean.com, and a number of quarterly meetings, reports, condemnation data, and more. We encourage you to check out the new website, where you can access resources, sign up for our newsletter, and get updates and information related to OAHN and all species networks. Veterinarians can sign up for access to veterinary reports and educational content. We are also busy preparing for the annual DSP meeting on October 1, where vets, industry professionals, and members of government will come together to plan OAHN’s coming year.

The bee network held its latest quarterly conference call on March 9.

The OAHN alternative species network held its first conference call in July, with mink veterinarians discussing important issues with experts in the field. Main points of discussion for the call involved astrovirus and nursing sickness. To be added to the list for future calls, email oahn@uoguelph.ca.

The Canadian Wildlife Health Cooperative will be creating a report on wildlife disease surveillance (expected release date: fall 2015).

We had 71 responses to the Q1 veterinary survey for bovine practitioners. The quarterly call occurred in May and the resulting report was disseminated to the OABP listserv at the end of May. AHL data and condemnation data were also included. The Q2 survey has been sent to practitioners, with a conference call scheduled for August.

The first OAHN bee network meeting took place in June, with members from OBA, Tech Transfer, research, AHL and OMAFRA. Check out our OAHN bee podcast, released on August 6. In the podcast, Dr. Jennifer Zechel discusses bee health, testing, and common misconceptions about bees.

The OAHN swine network completed its Q2 2015 veterinary survey and had its quarterly conference call in July. The main points of concern discussed on the call were: influenza A typing, PEDV, porcine deltacoronavirus, swine dysentery, and HEV. Watch for the swine veterinary report and producer report to be published on OASV listserv and on OAHN.ca in the coming month.

The Q2 equine veterinary report was released to the OAEP listserv and posted on OAHN.ca in July. The top concerns discussed during the Q2 conference call were: uterine infections, angular limb deformities, and neonatal diarrhea in foals and breeding stock; and pastern dermatitis, RAO/heaves, and laminitis in adults. IDEXX laboratories and the AHL contributed laboratory data for this quarter.

The Q2 2015 veterinary survey was completed and the quarterly conference call occurred in the second half of July. Look out for the veterinary and producer reports on the SRVO listserv and on OAHN.ca in the near future. Top items of discussion were: coccidiosis, listeriosis, and clostridial enteritis.

The Q2 2015 (Feb/March/April) meeting took place in May, and the producer report was disseminated and is available on OAHN.ca. Top issues for discussion during the Q2 conference call included: infectious bronchitis virus, lameness, and systemic bacterial infection. The Q3 2015 survey is now available and was sent out on the OAPP listserv. The Q3 poultry conference call will take place in early September, with producer and veterinary reports to be released shortly thereafter. A representative from OAHN will be at the OAPV meeting on September 9.

The OAHN Fish Network had its 3rd quarterly conference call and welcomed 2 representatives from industry group NOAA, and 2 veterinarians from CFIA. The network will have its third quarterly call this fall.

The companion animal network has chosen its 3 veterinarian representatives. There were many impressive applicants, and the advisory team chose Dr. Susan Little as the Eastern Ontario rep, Dr. Emma Webster as the Southwestern Ontario rep, and Dr. Hailey Bertrand as the Northern Ontario rep. We will be sending out the first companion animal survey in September, with a conference call following. Look for the first OAHN companion animal reports this fall.
RUMINANTS
Tissue sampling and test selection for field PMs
Josepha DeLay, Jan Shapiro, Maria Spinato, Andrew Brooks
The type and quality of samples submitted to the diagnostic laboratory has a tremendous impact on the diagnostic information that you (and your client) will glean from testing. Your clinical and postmortem differential diagnoses will determine test selection for each case. Plan ahead for those tests that will likely be necessary, and know which specific samples are required for each test. Remember that tissues fixed in formalin are suitable only for histopathology and immunohistochemistry. Microbiologic tests require fresh tissue; frozen tissue may be substituted, if available. The general guidelines listed below for sampling are based on common, specific clinical conditions.
Diarrhea
Intestinal samples will obviously be important, and careful handling is required to prevent contamination of other tissues. For microbiologic testing, fresh intestinal segments 5-10 cm long should be placed into labelled whirl-pak bags. Feces may be collected in sterile screw-top containers.
General sample requirements:
· 1 sample of small intestine (jejunum or ileum) and colon for bacterial culture
· 1 sample of small intestine (jejunum) and colon for various viral/bacterial PCRs (dependent on species/age group)
· 1 fecal sample for parasitology
· multiple (6-10) samples from intestine for histopathology, including all levels of the intestinal tract and stomach (in formalin).
Optimal fixation will occur if the intestinal loop is opened longitudinally before placing in formalin (rather than fixing cross-sectional ‘doughnuts’ of intestine). For neonatal piglets, pups, and kittens, this is nearly impossible, and the thin-walled intestinal segments may be fixed intact (no opening necessary).
Example of sampling and testing for bovine neonatal diarrhea:
· Bacterial culture (SI / ileum and colon)
· Bovine coronavirus and ruminant rotavirus PCR (SI / jejunum and colon)
· Sucrose wet mount for Cryptosporidium (feces)
· Histopathology (multiple intestinal samples as above; also include mesenteric lymph node, forestomachs, abomasum, lung, thymus, heart, liver, spleen, kidney, adrenal gland, and skeletal muscle – to evaluate for other neonatal conditions including septicemia and nutritional myopathy)
Pneumonia
Lung is a large organ, with regional variation in susceptibility to various infectious agents. Samples should be taken using a clean scalpel blade, and placed in separate, labelled whirl-pak bags.
General sample requirements:
· 3 approximately 5 X 5 cm samples from the margin of affected and unaffected lung for bacterial culture, mycoplasma PCR, and viral PCR
· bronchial lymph node, trachea, heart, and 3 samples from each of cranial, middle, and caudal lobes of lung, and including the margin of affected and unaffected lung, for histopathology.
Example of sampling and testing for bovine pneumonia:
· Bacterial culture (lung, at margin of lesion and normal tissue)
· Mycoplasma bovis PCR (lung, at margin of lesion and normal tissue)
· BRSV, IBRV, PI-3, +/- BVDV PCR (lung, at margin of lesion and normal tissue)
· Histopathology (multiple samples as above)
Unexpected death with no gross lesions on PM
Sampling should include a wide range of tissues for histopathologic examination. A similar range of tissues should be frozen for potential microbiologic and / or toxicologic testing, based on histopathology results. Brain and heart are especially important. Head may be submitted to the diagnostic lab intact for brain removal, if desired. Heart may also be submitted intact for gross examination.
Histopathology: BRAIN (1 half of sagittally sectioned brain), HEART (left papillary muscle, interventricular septum, right ventricular free wall), lung x3 (cranial, middle, and caudal lobes), thyroid gland, thymus, kidney (include cortex and medulla), adrenal gland, pancreas, liver, spleen, mesenteric lymph node, skeletal muscle, gastrointestinal tract (1 section from each of forestomachs, stomach / abomasum, duodenum, jejunum, ileum, colon, rectum).
Freeze the following tissues, each in separate labelled whirl-pak bags: brain (half of sagittally sectioned brain), heart (left ventricle), lung (cranial lobe), kidney, liver, spleen, ileum, colon. Approximately 5 cm diameter samples from solid organs are appropriate.
**Also include STOMACH CONTENT and URINE among the samples to freeze. Each may be collected in a sterile screw-top container.
Additional information on PM methods and procedures, tissue sampling, and sample submission to the AHL can be found at the following links:
Tips for Practitioners for Field Postmortems https://www.uoguelph.ca/ahl/ahl-labnote-2-tips-practitioners-field-postmortems
Field and Clinic Postmortems: Simplified Protocol and Image List https://www.uoguelph.ca/ahl/ahl-labnote-42-field-and-clinic-postmortems-simplified-protocol-and-image-list
Brain Removal in Field Postmortems https://www.uoguelph.ca/ahl/ahl-labnote-33-brain-removal-field-postmortems
Submission Instructions https://www.uoguelph.ca/ahl/submissions/ahl-labnote-27-submission-instructions
Additional information on sampling and test selection information for specific disease conditions in various species can be found in the AHL Users’ Guide – Disease Investigation section: http://www.guelphlabservices.com/AHL/UsersGuide.aspx
Salmonella Dublin update
Durda Slavic, Andy Vince, Jim Fairles
Salmonella enterica ssp. enterica serovar Dublin is considered a host adapted Salmonella of cattle. It can affect cattle of all ages but it is usually more severe in younger, immunologically ‘naive’ animals. Calves can be infected at calving but do not necessarily show any clinical signs until they are 2-3 weeks old. In general, S. Dublin disease is most frequently reported in cattle over 3 months of age.
Lesions caused by S. Dublin usually differ from lesions caused by other Salmonella serotypes. S. Dublin more consistently results in septicemia in young calves, and less consistently in necrotizing enteritis.
Frequently, lesions include:
· multifocal necrotizing hepatitis and splenitis (but without producing the inflammatory “paratyphoid nodules” seen with other strains);
· arthritis (often involving the growth plates of long bones);
· bronchopneumonia;
· dry gangrene of the distal limbs, tail, and ears;
· abortion is common in endemic areas.
Although S. Dublin has been causing problems in cattle in the northeastern United States and in the Prairies for years, the first case detected in Ontario by our laboratory was in December of 2012. Since then, the bacteriology laboratory has been screening all bovine lungs submitted for culture and susceptibility for the presence of this pathogen through an enrichment method. No S. Dublin was detected in 2013. There was one veal operation with the clinical presentation of diarrhea and pneumonia in 6-8 week-old Holstein calves diagnosed with S. Dublin in 2014. To date in 2015, S. Dublin has been detected in 3 veal operations (2 new sites, and 1 from 2014). Multiple cases were received from these operations and the clinical history indicates that these animals predominantly suffer from pneumonia that is not responsive to treatment. In addition, these animals usually come from multiple sources including other Canadian provinces where cases of S. Dublin are on the rise.
Given that S. Dublin has been identified in Ontario, we recommend adding S. Dublin to a differential diagnosis for cases of septicemia and respiratory problems in young calves, particularly in veal operations.
The AHL bacteriology laboratory continues to screen all bovine lungs for the presence of S. Dublin and will start reporting results for routine submissions. If Salmonella sp. is isolated from lungs or from any other internal organs on primary culture, then serogrouping for group D Salmonella will be also reported. S. Dublin belongs to group D Salmonella but it is not the only member of group D. Therefore, isolation of group D Salmonella does not necessary means that it is S. Dublin, but in combination with clinical history it may be highly suggestive. All Salmonella isolates from the AHL are sent to the Public Health Agency of Canada for confirmation of serotype.
Bovine coronavirus (BCV) and rotavirus (BRV) – on the increase?
Murray Hazlett, Davor Ojkic, Josepha DeLay, Jim Fairles
A subjective increase has been noted in the number of bovine coronavirus (BCV) cases submitted to the AHL. This may in part be the result of better testing - we no longer rely on the bovine coronavirus ELISA, or the rotavirus A latex agglutination test (RLA) - these have been replaced by polymerase chain reaction (PCR) and immunohistochemistry (IHC) testing.
Figure 1 illustrates the percentage of positive bovine submissions by quarter for both coronavirus (blue) and rotavirus (red). It shows a dramatic increase in both the number of submissions that had at least one positive test (of any sort) for either bovine coronavirus or bovine rotavirus. For bovine rotavirus (BRV), this started in the first quarter of 2013, with a marked increase starting in 2014 Q1. For bovine coronavirus, this started in 2014 Q1 and continues to escalate. Our PCR tests for bovine coronavirus and bovine rotavirus were both instituted in late 2012 and our IHC for bovine coronavirus in 2007, so the dramatic increases do not seem to correlate with improved testing.
During this period, if a positive coronavirus submission was also tested for rotavirus, it had a 55% chance of being positive for both. Most of the rotavirus identified by PCR was type A (224 cases) with only 4 rotavirus B cases.
The data suggest an increase in both bovine coronavirus and bovine rotavirus cases among AHL submissions. Figure 2 shows the percent positive of cases tested for BRV by year and the percent positive of cases tested for bovine coronavirus by year. It shows an increase for both BRV, with a spike in 2013, and BCV, with a spike in the first two quarters of 2015. The rotavirus spike shown in Fig 1, 14-3 and 14-4, is likely the result of increased testing.
In the winter of 2014, we identified 2 cases that were strongly IHC positive for coronavirus (Fig. 3) but were PCR negative, and the primer was modified to identify the strain in these samples and to improve test sensitivity. This occurrence may have represented either a new strain of coronavirus, or simply that we were better at IHC testing, however an increase in positive BCV PCR tests was happening before this event.
While it does appear that the AHL is seeing more cases of BCV this year, this may not reflect the “real world” situation regarding BCV and BRV, as there may be other factors influencing lab submissions.
|
|
|
|
|
Figure 1. Percent positive bovine submissions by quarter, 2009 4th quarter to 2015 2nd quarter. There were totals of 208 BCV positive submissions and 233 BRV positive submissions. |
Figure 2. Percent of tests that were positive by year. |
Figure 3. Strong positive IHC staining for bovine coronavirus antigen in colon from a calf that was BCV PCR negative, showing the value of using more than one test for diagnostic evaluation. |
SWINE
Brachyspira testing update
Durda Slavic
The AHL currently offers culture and real-time PCR (rt-PCR) detection of Brachyspira spp. Culture is done on request only; it is time consuming, and one week notice to the lab is recommended because selective media need to be made. In contrast, rt-PCR can be done within a day or two and no advance notification is required. More importantly, in our hands rt-PCR appears to be more sensitive than culture.
Since 2013, 93 samples were tested in the AHL bacteriology section by culture and PCR for the presence of Brachyspira spp. We tested 64 fecal samples and 29 tissue samples. For culture, we used 2 different selective media and 2 different incubation temperatures (37° C and 42° C). For rt-PCR, Brachyspira spp. was detected by using a genus-specific probe whereas species-specific probes were used to detect Brachyspira hyodysenteriae, Brachyspira pilosicoli, Brachyspira hampsonii clade I, and B. hampsonii clade II. Of 64 fecal samples, 23/64 (34%) were positive for the presence of Brachyspira spp. by rt-PCR, whereas only 9/64 (14%) samples were positive on culture. All fecal samples that were positive on culture were also positive on PCR. In total, 29 tissue samples were tested and only 3/29 (10%) samples were positive on both PCR and culture. The rest of the samples were negative by both methods. Based on these limited data , it appears that our rt-PCR will detect Brachyspira spp. in 20% more fecal samples than culture. No differences were observed for tissue samples, but that could be attributed partially to the smaller sample size.
To confirm that our samples are truly positive for the presence of Brachyspira spp., we attempted sequencing of rt-PCR products from the randomly chosen 12 positive samples. Six of these samples were positive for Brachyspira spp. by both culture and rt-PCR and 6 samples were positive by rt-PCR only. All sequencing was done on PCR products obtained from nucleic acid extracted from original samples (e.g., feces and tissue). The sequencing results confirmed the presence of Brachyspira spp. in all 12 samples, but in 6 samples more than 1 species of Brachyspira appeared to be present.
To further explore the robustness of our rt-PCR and to resolve issues with a mixed Brachyspira population being present in the samples, 17 samples were randomly chosen for next generation sequencing by the GS Junior. The advantage of this type of sequencing over gel-based sequencing is that it can detect multiple species of Brachyspira in the same sample simultaneously. The results of next generation sequencing were then compared to the individual rt-PCR results, which included results for 5 different Brachyspira spp. (Table 1). There was good agreement between GS Junior sequencing and our rt-PCR results.
For diagnostic purposes, our Brachyspira panel is used for detection of Brachyspira spp. at the genus level and B. hyodysenteriae, B. pilosicoli, B. hampsonii clade I, and B. hampsonii clade II at the species level. If samples are positive for Brachyspira spp. at the genus level but negative for pathogenic species currently tested, it is most likely that other species of Brachyspira of questionable clinical significance are present, such as B. murdochii, B. intermedia, or B. innocens. If submitting samples for culture, please call the laboratory a week in advance to allow time for selective media to be made.
Table 1. Comparison of next generation sequencing (GS Junior) and rt-PCR results. POS=positive, ND=not detected, INC=inconclusive.

AVIAN/FUR/EXOTIC SPECIES

Do you have small flock poultry clients? OMAFRA and U of Guelph, through the Animal Health Lab and the Ontario Animal Health Network are starting a small flock disease surveillance project October 1st. Non-quota, non-commercial poultry owners can submit cases through their veterinarian at the rate of $25 per case. In exchange, the owner will need to complete a survey.
Click below for more details:
COMPANION ANIMALS
Update on Echinococcus multilocularis in Ontario
Emily Brouwer, Andrew Peregrine, Andrew Vince
In the March 2013 issue of the AHL Newsletter, Dr. Brooks et al. described a case of hepatic Echinococcus multilocularis infestation in a 2-year-old Boxer dog. Since that time, 3 additional cases have been identified in dogs by the OVC Department of Pathobiology and the Animal Health Laboratory from within Southern Ontario, a region in which this pathogen had not been previously identified.
Very recently, a 4-year-old male castrated Boxer dog was presented to the OVC Health Sciences Center with lethargy, vomiting, abdominal pain, and radiographic findings of a cranial abdominal mass. Clinical pathology on admission included severe leukopenia, neutropenia, and mild lymphocytosis. Analysis of free abdominal fluid revealed septic suppurative inflammation. On exploratory laparotomy, 3 large cavitated masses were identified in the liver varying from 10-25cm in diameter; 2 were amenable to surgical excision and submitted for histopathology (Fig. 1). These masses were filled with tan purulent fluid and had coalescing white nodules within their wall; histologically, the wall of each mass contained a mix of granulomatous and neutrophilic inflammation surrounding multilocular cysts lined by PAS-positive hyaline membranes, and occasionally contained calcareous corpuscles and cross sections of protoscolices (Fig. 2). The diagnosis of Echinococcus multilocularis was confirmed using PCR and sequencing at the Institut für Parasitologie in Bern, Switzerland.
Overall, 3 cases of abdominal visceral and 1 case of subcutaneous Echinococcus multilocularis infestation have been identified recently in Ontario dogs, comprising 3 Boxer dogs and 1 Leonberger. Only one case had a history of travel outside of Ontario. Visceral infestations are uncommon in canids, which are typically definitive hosts with infestations limited to the intestinal tract; visceral infestations typically result from ingestion of large numbers of parasite eggs, most likely in the feces of wild canids. Because of the tendency to produce multifocal and often dramatic masses, alveolar echinococcosis should be considered a differential diagnosis for intraabdominal neoplasia in dogs.
This pathogen is of significant public health interest, as Swiss studies have demonstrated that approximately one-third of canine visceral cases also have enteric infections; as such, it is considered likely that more cases will be seen in Ontario. Canine enteric infections are potentially infectious to humans in close contact; human cases are typically visceral, mimic neoplasia, and have a high case fatality if not treated (particularly when diagnosed late). Dogs and people in contact with infected dogs are typically screened serologically for exposure.
Bayer Animal Health is funding an MSc research project beginning in September 2015, which will investigate levels of infestation within hunter-trapped foxes and coyotes (the typical definitive wildlife hosts for this parasite) across southern Ontario.
For additional information on this parasite, a YouTube video presentation by Dr. Andrew Peregrine is available at: https://www.youtube.com/watch?v=XSss8BaD7Lg&feature=youtu.be
|
|
|
|
Figure 1. Intraoperative photograph of liver masses with characteristic military pale surface nodules (Dr. Tom Gibson, Ontario Veterinary College, with permission). |
Figure 2. Histology from the wall of one of the resected masses, with two protoscolices from encysted tapeworms (H&E, 400x magnification). |
Minimal inhibitory concentration (MIC) of minocycline in treatment of Staphylococcus pseudintermedius
Durda Slavic
The AHL has been reporting minimal inhibitory concentration (MIC) for minocycline for all methicillin-resistant Staphylococcus pseudintermedius (MRSP) isolates. Although minocycline has not been officially approved for use in dogs, it can be a good alternative in treating multidrug resistant (MDR) MRSP. Maaland et al. determined pharmacokinetic and pharmacodynamic data for minocycline in dogs. Minocycline, when used twice daily at the dosage of 5 mg/kg, will inhibit growth of S. pseudintermedius isolates with MIC values of ≤0.25 μg/mL. Furthermore, it has been shown that S. pseudintermedius isolates with MIC ≤0.25 μg/mL do not carry any currently known tetracycline resistance genes, unlike their counterparts with MIC values above 0.25 μg/mL.
“Urinalysis is one of the most important diagnostic tools available to veterinarians.” (Dr. Carl Osborne, Urinalysis: A clinical guide to compassionate patient care)
Kris Ruotsalo
Without information obtained by a comprehensive urinalysis (which includes dipstick, specific gravity, and sediment examination), many of the changes noted on serum biochemistry profiles or clinical assessment cannot be adequately interpreted. For example, urine specific gravity is helpful in differentiating the cause of azotemia, urinary protein loss may account for documented hypoproteinemia, and hyposthenuria may be related to an underlying urinary tract infection, etc.
Even the absence of significant findings is helpful, providing the veterinarian with objective information with which to exclude certain disease processes. As such, a urine sample should be part of the minimum data base, evaluated alongside every serum biochemistry profile and CBC, whenever it is clinically possible.
In order to maximize the information obtained from urinalysis, a standard protocol should be established, keeping the following points in mind:
* Perform the urinalysis when urine is at body or room temperature. If urinalysis cannot be performed within approximately 30-60 minutes of sample collection, refrigeration is indicated. While some things are best when cold and straight from the fridge, urine is not one of these!
* Enzyme-based tests such as glucose oxidase, require urine to be at room temperature.
* The specific gravity of urine is higher in cold urine than warm.
* Precipitated substances are more likely to re-dissolve in samples that have been rewarmed.
* Determine urine specific gravity using a veterinary specific refractometer.
* Keep the urine dipstick container cap on tightly, ensure that the desiccant is in place, and store the container away from moisture, direct sunlight, heat, acids, alkalis, and volatile fumes. Do not use outdated reagents. Commercially available control material (e.g., Dipper Quantimetrix Corp) is available to check dipstick quality.
* Do not interpret the nitrite, leukocyte, or specific gravity pads, these are not reliable in animal species.
* Minimize contamination of reagents from one test pad with reagents from an adjacent test pad by keeping the reagent strips horizontal after the application of urine.
* Evaluate the test results at the times specified by the manufacturer.
Do examine a urine sediment preparation. If using a sediment stain, periodically examine the stain itself to ensure that is has not become contaminated by bacteria or yeast.






